An overview of hormone-free contraceptive alternatives
Headaches, loss of libido, depressive moods: The list of side effects of hormonal contraceptives such as the pill or the hormonal IUD is long. However, hormone-free alternatives can be just as effective and are also free from these side effects. But beware: Not all well-known methods are suitable for reliable contraception. Therefore, you should inform yourself thoroughly to make an informed decision about your method of contraception. In this article, you will learn everything about hormone-free contraception methods: what methods and terms exist, how to use them, and how safe they really are.
How can I prevent pregnancy without hormones?
Contraception using hormonal methods, such as the hormonal IUD, the birth control pill, or the contraceptive patch, significantly interferes with your hormone balance and alters physiological processes. They suppress the natural cycle, preventing ovulation and thus pregnancy.
Therefore, those who want to switch to hormone-free contraception face the question: How can I prevent pregnancy if ovulation has already occurred? How reliable can this method be? And how do I know when I’m fertile? We would like to answer these questions for you and give you the confidence you need.
Contraception with barrier methods
Barrier methods ensure that sperm are physically prevented from entering the uterus. These methods include condoms and diaphragms, for example. Depending on the contraceptive method, it is used once by the woman or the man during each sexual intercourse.
The Condom
Condoms are one of the few contraceptive methods that protect against both pregnancy and sexually transmitted infections. They are usually made of latex and must be used every time you have sex. For men, condoms are thin protective sheaths that are slipped over the erect penis, while the female condom is a bag that is inserted into the vagina.

To ensure that condoms protect effectively, correct use is crucial:
When using condoms for men, the correct size should be chosen, and the condom must be rolled onto the penis before any genital contact occurs. It is important to leave about 1.5 cm of space at the tip for the semen and to press out any trapped air. After ejaculation, the penis should be withdrawn immediately, holding the condom at the base of the shaft to prevent it from slipping off or leaking.
Female condoms consist of a pouch with an inner and an outer ring. The inner ring is inserted deep into the vagina, while the outer ring remains outside. The penis is then guided through the outer ring into the pouch. After intercourse, the outer ring of the female condom should be compressed and twisted to prevent semen from leaking out. The condom can then be carefully removed.
Costs: Female condom: approximately €4 per piece, male condom: less than €1 per piece
The Diaphragm
The diaphragm is a contraceptive method in which a dome-shaped rubber cap with a flexible rim is inserted into the vagina to cover the cervix and prevent sperm from entering the uterus. Diaphragms come in various sizes and should be fitted by a healthcare professional. During this process, the woman is shown how to correctly insert the diaphragm so that it fully covers the cervix without causing discomfort. Neither the user nor her partner should feel the diaphragm during intercourse.

In addition to traditional diaphragms made of latex, there are also newer models made of silicone. These are softer, more durable, and often available in a one-size-fits-all design, making them easier to use.
It is important to use the diaphragm in combination with a spermicide to increase contraceptive effectiveness. A spermicide is a substance that kills sperm or inhibits their mobility and is applied to the inside of the diaphragm. The diaphragm can be inserted up to 2 hours before intercourse and should remain in the vagina for at least 6 to 8 hours afterward but no longer than 24 hours. Diaphragms can be washed and reused but should be regularly checked for tears.
Costs: €31–€38 for one-size models, €50–€70 for models available in various sizes.
Contraception with Copper: The Copper Intrauterinpessar (IUD) and the Copper Chain
Copper acts as a contraceptive method by impairing the mobility of sperm, preventing fertilization even if ovulation occurs. Additionally, copper disrupts the buildup of the uterine lining, preventing the implantation of a fertilized egg in the uterus. Furthermore, the released copper ions alter the cervical mucus in the cervix, blocking the sperm’s path to the egg. There are two main forms of copper contraception: the copper IUD and the copper chain.

The copper IUD is a small T-shaped plastic device wrapped with copper wire and inserted into the uterus. The copper chain is a contraceptive method made up of several copper tubes strung on a nylon thread and anchored in the upper uterine muscle using a needle. Both the copper IUD and the copper chain work as contraceptives by releasing copper ions into the uterus, which impair the mobility and fertilizing ability of sperm and prevent the implantation of a fertilized egg.
The insertion and removal are performed by a gynecologist. The doctor inserts the IUD or the copper chain through the vagina and cervix into the uterus. The insertion can be painful or painless, depending on individual factors such as pain sensitivity and the doctor’s experience. Local anesthesia or pain medication may help.
The removal is done by gently pulling on the retrieval threads and may be associated with mild, short-term pain. The IUD or copper chain should be regularly checked by a doctor and removed or replaced if necessary.
The copper IUD and copper chain are very effective contraceptive methods. However, due to the insertion procedure and the effect of copper in the body, unwanted side effects may occur:
– Increased menstruation: Especially in the first few months, bleeding may be heavier, and period cramps may become more intense.
– Spotting: This can also occur in the first few months but often subsides over time.
– Infection risk: In the first few weeks after insertion, there is a slightly increased risk of infections in the uterus or fallopian tubes, especially if sexually transmitted infections are present.
– Injuries: Very rarely, the insertion can cause injury to the uterine wall, particularly if the IUD or copper chain is inserted immediately after childbirth or if there is an unusual uterine position.
– Displacement: In the first 12 months, the IUD or copper chain may become dislodged and slip out. This occurs in about 5 out of 1,000 women.
The insertion of copper should therefore be carefully considered, as this contraceptive method is suitable for long-term use, ranging from 3 to 10 years — with the latter involving a higher copper dosage.
Costs: 350 – 500€
Contraception with Gold: The Gold Intrauterinpessar (IUD)
The gold IUD differs from the copper IUD in fewer ways than its name might suggest. This contraceptive method also uses a wire that wraps around the T-shaped plastic body. However, the wire is made of a gold-copper alloy, and some models use a gold core with a copper wire. The gold content of the IUD does not affect its contraceptive effectiveness – this is still achieved by the copper ions. The gold’s purpose is to extend the durability of the copper wire and provide protection against infections. However, this protection against infections has not been proven. Like the copper IUD, the gold IUD is inserted into the uterus and can therefore have the same side effects from insertion by a doctor and the same mechanism of action through copper ions. If a user has issues with contraception using copper, the gold IUD is not a suitable alternative, even though its name might suggest otherwise.
Costs: 140 – 350€
Natural Family Planning or Natural Contraception
Natural contraception is often referred to as „Natural Family Planning“ (NFP), as it can be used both for contraception and to fulfill a desire for children. NFP is based on reliably determining the fertile days around ovulation in the cycle. On fertile days, additional protection or abstinence from vaginal intercourse is necessary, while on infertile days, intercourse can occur without additional contraception.
Natural contraception therefore comes without any side effects and at little to no cost.
In the following sections, we provide an overview of hormone-free contraceptive methods, their effectiveness, as well as their advantages and disadvantages.
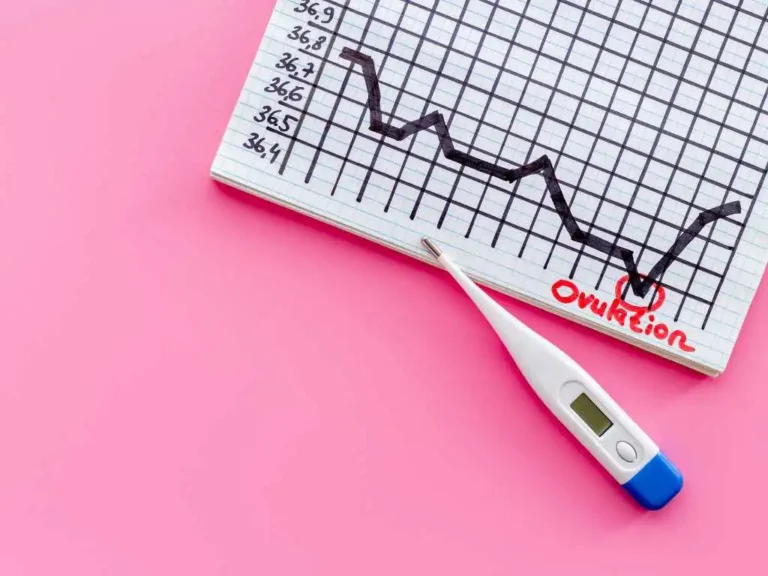
The Sympto-Thermal Method
With the symptothermal method, you determine your ovulation based on two independent bodily signs: your basal body temperature pattern and the quality of your cervical mucus. These two parameters reliably change throughout the cycle, providing clear indications of whether ovulation has occurred and the fertile phase has ended or not. Because two parameters are monitored, there is also double confirmation. The method has been scientifically proven in multiple studies and, with a Pearl Index of 0.4, is just as effective as the pill. You can learn how to use the method here.
With trackle, you use contraception according to the rules of the symptothermal method. It is considered the safest method in natural family planning and has been officially recommended as a reliable contraceptive method by the German Society for Gynecology and Obstetrics (DGGG) since 2024. trackle makes the application digital and straightforward, eliminating the fear of making mistakes.
The Temperature Method
You’ve probably heard of contraception using the temperature method. As the name suggests, the temperature method relies solely on evaluating your body temperature and does not consider any additional fertility indicators, such as cervical mucus. This makes it significantly less reliable than the symptothermal method, as temperature alone can be highly susceptible to disruptions. Even combining it with calendar-based methods does not make the temperature method more reliable – but more on that shortly.
The Billings Method – also known as the Cervical Mucus Method
Throughout your entire cycle, the consistency of cervical mucus changes. The Billings Method takes advantage of this. With this method, you observe your cervical mucus daily and record it in a chart to detect any changes. However, cervical mucus alone is not sufficient to draw conclusions about your fertility during the cycle. While it can help identify the most fertile days if you’re trying to conceive, it is not suitable for reliable contraception.
The Calendar Method, Withdrawal Method & Co.: Caution, unreliable!
Right from the start: These methods are NOT recommended for reliable contraception, even though they are somewhat widespread. In reality, they are very unreliable and therefore not suitable for contraceptive purposes.
The Calendar Method
The calendar method involves calculating the infertile period in the female cycle. For this, past menstruations are carefully recorded. The fertile and infertile days are then calculated based on the lengths of previous cycles.
Since ovulation can occur unexpectedly earlier or later due to various factors (e.g., illnesses, medications, or stress), this method is highly unreliable and not recommended. Apps that rely solely on cycle data, such as the menstrual period, are also unsuitable for contraception. The user reliability of the calendar method is 20, meaning that more than 1 in 5 women using this method typically become pregnant. The idea that ovulation can be reliably calculated is therefore a persistent myth.
Coitus interruptus
Coitus interruptus, „pulling out,“ or „pull and pray“ – whatever you call it, this is an unreliable method of contraception where the man withdraws his penis from the vagina before ejaculation. Although it may seem straightforward to apply, it requires not only a high level of self-control but also offers insufficient reliability. Pre-ejaculate fluid, for example, can contain sperm that may lead to pregnancy even before climax. Similar to the calendar method, the user reliability of coitus interruptus is 22. So once again: a clear recommendation NOT to rely on coitus interruptus as a contraceptive method!
Ovulation Tests
Ovulation tests (also called LH tests) work similarly to pregnancy tests: you urinate on a test strip, which indicates whether your luteinizing hormone (LH) levels are elevated. A positive result signals that ovulation may soon occur. However, these tests are entirely unsuitable for contraception because various factors (e.g., the time of day or fluid intake) can influence LH concentration in urine, leading to unreliable results. Additionally, some women experience multiple LH surges per cycle, meaning an LH surge cannot precisely predict or confirm ovulation.
Yam Root
Now it gets wild: On social media, some young women have reported using yam root as a natural contraceptive. The idea stems from claims that the indigenous peoples of the Americas supposedly used yam root for contraception. This is based on the fact that diosgenin, a compound found in yam root, was indeed a precursor for the first birth control pill. But beware: eating the tuber itself does not provide contraception, as diosgenin must be converted into progesterone in a lab. Whether the body can convert diosgenin on its own is unclear. Moreover, there are no studies confirming yam root as an effective contraceptive. On the contrary, the plant is said to boost fertility in women – though this, too, has not been scientifically proven.
Hormone-Free Contraception – Your Choice
Hormone-free contraception works differently from what you might know from taking the pill. It involves understanding your body’s processes, your fertility, and your sexuality. Additionally, hormone-free contraception always involves two people—a basic understanding of the menstrual cycle is essential. But don’t worry: it’s not as complicated as it sounds! In fact, it’s incredibly fascinating because you’ll get to know and understand yourself and your body better. trackle uses the safest method of natural family planning and helps you apply a well-researched, scientifically backed method in a simple and digital way. This cycle tracker makes hormone-free contraception as easy and reliable as possible. Learn more here about how trackle works.
Sources:
Diedrich, K. et al.: Gynaecology and Obstetrics. 2nd edition. Heidelberg. 2007
Frank-Herrmann, P. et al.: Natural Family Planning Today. Modern Cycle Knowledge for Counseling and Application, 6th edition. Heidelberg, 2020
Barrier Methods. MSD Manual –> https://www.msdmanuals.com/de-de/heim/gesundheitsprobleme-von-frauen/familienplanung/barrieremethoden#Spermizide_v8951509_de
Contraceptive Methods. Federal Centre for Health Education –> https://www.familienplanung.de/verhuetung/verhuetungsmethoden/
Yam Root. Netdoktor –> https://www.netdoktor.de/heilpflanzen/yamswurzel/
Ovulation Test. Netdoktor –> https://www.netdoktor.de/kinderwunsch/ovulationstest/
Contraception – Unreliable Methods. University Hospital Tübingen – Department of Women’s Health –> https://www.medizin.uni-tuebingen.de/de/das-klinikum/einrichtungen/kliniken/frauenklinik/jugendgynaekologie/verhuetung/unsichere-methoden
Gold IUD. Raxal GmbH –> https://www.kupferspirale.info/goldspirale
