Contraception for men
In our society, the responsibility for contraception often lies with women. However, it is no longer a woman’s responsibility to avoid an unwanted pregnancy, which, as we know, always involves two people. Contraception for men is becoming increasingly important.
The mere fact that a woman’s fertile window in her cycle is a maximum of 18 hours, while men are fertile every day with the continuous production of sperm, allows a different perspective on the topic of “male contraception”. Incidentally, when these two criteria are combined, we arrive at a combined fertility of a maximum of seven days in the female cycle.
So it’s high time we took advantage of these scientifically proven facts and questioned whether women really need to burden their bodies with artificial hormones or copper on a daily basis. If your answer to this question is already “no”, you’ve come to the right place:
In this article, you’ll find out which male contraceptive methods are available, which of them are really safe and which you’re better off staying away from if a high level of contraceptive safety is important to you. We also look at the side effects and introduce you to an additional option for shared contraception.

Contraception for men - these are the safe options available:
While there are a variety of known contraceptives for women, there are only two safe methods available for male contraception:
- The condom (barrier method)
- Vasectomy (surgical measure)
The condom
The condom is the most popular contraceptive among Germans, according to a study conducted by the Federal Center for Health Education (BZgA) in 2023. For the first time, the condom even overtook the contraceptive pill, which had been in the lead up to this point.

The condom is the best-known and most commonly used contraceptive method for men and is usually made of latex. However, there are also plastic condoms that offer a suitable alternative for people with latex allergies. They are put over the erect penis before sexual intercourse and prevent sperm from entering the vagina. A major advantage of condoms compared to other contraceptives is protection against sexually transmitted diseases.
When used correctly, condoms are quite safe, as they have a Pearl Index of two. The Pearl Index is a unit of measurement that indicates the safety of a contraceptive method. It indicates how many out of 100 users became pregnant over the course of a year despite using this contraceptive method. A low Pearl Index therefore means greater safety.
However, to ensure maximum safety, it is important to wear the condom throughout sexual intercourse and to choose the right size. The storage of condoms is also crucial: they should not be exposed to heat or direct sunlight, including body heat and friction that can occur in a trouser pocket or purse. It is also important to note the expiration date and ensure that the packaging is undamaged to guarantee the effectiveness of the condom.
Vasectomy
Vasectomy is a long-term method of contraception, particularly suitable for men who do not wish to have children or who have completed their family planning. There are various methods for performing the surgical procedure: often, a small incision is made in the scrotum to cut the vas deferens and seal the ends, so that although the testicles continue to produce sperm, it is no longer detectable in the ejaculate. Neither libido nor potency is affected by the procedure, despite this being a common misconception. Vasectomy is only effective after several weeks, so other methods of contraception must be used during this time.

Compared to sterilization in women, vasectomy is significantly simpler and less risky. Although it is generally considered an irreversible procedure, it can be reversed in approximately 60–95% of cases. While its effectiveness is ensured by a very low Pearl Index of 0.05, reversibility is not guaranteed, which is why young men are often advised against this method.
You'd better stay away from that:
Coitus interruptus
Coitus interruptus, also known as the „withdrawal method“ or „pulling out,“ is an unreliable method of contraception in which the man withdraws his penis from the vagina before ejaculation. Although the withdrawal method is easy to use and requires no preparation or aids, a high degree of self-control is necessary. Generally, the method does not offer sufficient protection, as seminal fluid, for example in the form of pre-ejaculatory fluid, can be released even before climax. Ejaculation immediately outside the vaginal opening can also lead to pregnancy. The failure rate for coitus interruptus is 22 – meaning that with typical use, more than one in five women will become pregnant using this method.
The pill for men
The so-called „male birth control pill“ is not yet available. Despite numerous studies that have investigated various options for hormonal contraception for men, none of the tested contraceptives have met the necessary criteria for approval.

The male contraceptive pill is intended to stop sperm production by suppressing hormones. However, previous studies with hormone preparations have highlighted the difficulties: side effects such as acne, weight gain, mood swings, depressive symptoms, and altered libido occurred in the test subjects, raising concerns about its tolerability. Some studies were even discontinued as a result. Since the side effects of the female contraceptive pill are comparable, these studies have sparked a debate about whether different standards of tolerability should apply to men and women – it is argued that under today’s approval criteria, the female contraceptive pill would likely not receive approval.
The male contraceptive pill therefore does not represent an adequate solution, but merely transfers the problems and side effects of hormonal contraception from women to men. Yet, there is the possibility of completely hormone-free contraception without side effects for both partners.
Natural family planning (NFP) - a safe, simple and side-effect-free method of contraception.
If you’re disappointed by the limited range of contraceptive options for men and are still hesitant about using contraceptives with side effects for your partner, we have a real alternative for you: Natural Family Planning (NFP) using the symptothermal method.
Unlike the pill or other hormonal contraceptives, the symptothermal method offers a shared, hormone-free method of contraception. It doesn’t interfere with your healthy bodily processes or those of your partner and has no side effects whatsoever.
Instead of placing the burden and potential risks solely on one partner, this method enables a collaborative and natural approach that strengthens understanding of the female cycle and fosters shared responsibility for contraception.

What is the symptothermal method and how reliable is it?
The symptothermal method (STM) was first described in 1965, has been scientifically validated multiple times, and is very well researched. This method precisely and accurately determines your partner’s fertile window, allowing you to either abstain from intercourse or use condoms on those days, while intercourse is safe without further contraception on non-fertile days. With a Pearl Index of 0.4, the symptothermal method is even as effective as the birth control pill, which has a Pearl Index of 0.3 to 1.
How does the symptothermal method work?
To find out when the fertile days in your partner’s cycle are, you need to determine when ovulation occurs. It’s important to note that sperm can survive in the female body for up to five days. Taking this survival time into account, along with the fact that the egg itself is only viable for a maximum of 18 hours after ovulation, and adding a small safety margin, results in a so-called „fertile window“ of up to seven days per cycle. Conception is impossible on all other days.
Caution: Reliably determining the fertile days is not possible using ovulation calculators, cycle calendars, or simple cycle tracking apps. This is because ovulation doesn’t always occur on the same day and must be determined anew in each cycle. What sounds complicated is actually made easy by the symptothermal method, which involves observing two different bodily signs.
In early 2024, the symptothermal method was even recommended by the German Society for Gynecology and Obstetrics (DGGG) in its guidelines for non-hormonal contraception as the only and safest method of natural family planning.

To determine ovulation, two independent bodily signs that have been proven to change cyclically are monitored daily: basal body temperature and cervical mucus (a type of healthy discharge that every woman has). While basal body temperature, also called resting temperature, rises by at least 0.2 degrees Celsius after ovulation, the consistency of the cervical mucus changes around the time of ovulation – it improves in quality, meaning that the cervical mucus becomes clear, glassy, and stretchy. Both bodily signs can be reliably observed and thus used to assess fertility status.
The reason for the changes in these bodily signs are the female hormones, which also trigger ovulation. This means they reliably indicate when ovulation is approaching and when it is definitely over. On the following cycle chart, you can see an example of how the temperature measurably increases after ovulation (shown in yellow here):
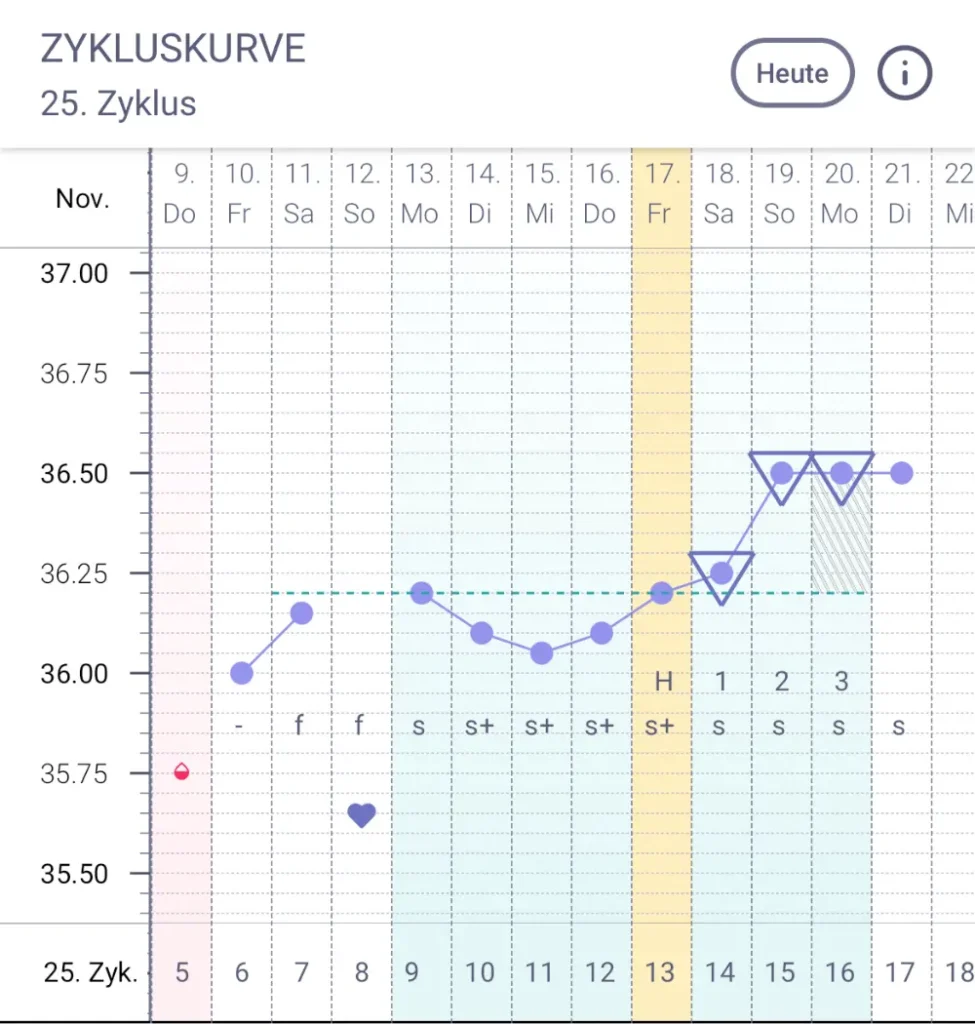
Now you’ve learned which physical signs your partner and you can use to determine when she is fertile and when she isn’t during her cycle. To correctly apply the symptothermal method, you now need to observe these two physical signs daily: Traditionally, the woman measures her basal body temperature every morning for three minutes after waking up and records her temperature reading and cervical mucus observations on a cycle chart. She then evaluates her fertility status, and you can both see each day whether she is fertile or not.
The only drawback, however, is that the fertility status has to be evaluated manually, and certain rules must be learned and followed. But we at trackle have the solution!
What advantages does trackle offer you?
trackle is a certified cycle tracker based on the rules of the symptothermal method, making the application of the method easy and digital for you in everyday life. The trackle sensor system is officially approved as a contraceptive device, just like the pill or the condom.
Using it is very simple: Your partner wears the sensor overnight and places it back in its case in the morning after getting up. There, it transmits her temperature data to the corresponding app. All that’s left is for her to record her cervical mucus observations, and you can then see her fertility status – so you know every day when your partner is fertile. Using trackle is not only super easy but also requires minimal time and effort to learn. The rules of the symptothermal method are always applied correctly, so there’s no need for daily entries in a cycle chart, manual evaluation, or external NFP (Natural Family Planning) counseling. Nevertheless, it’s helpful to familiarize yourself with the basics of the female cycle and the method to understand why natural contraception is truly effective in this way. Our free webinar can help you with this: Here you’ll get comprehensive knowledge about the cycle, the symptothermal method, and trackle – explained in a very simple and clear way.
If you have any further questions about our product, security, or data analysis, please don’t hesitate to contact our support team. We’re happy to help and will gladly tailor our assistance to your level of expertise. The best way to reach us is by email at info@trackle.de.
